As people age, physical changes are expected — but what about mental health? It’s a topic many families avoid or misunderstand, often brushing off signs of depression, anxiety, or memory loss in seniors as “just old age.” But the truth is: mental health matters at every stage of life, and that’s where geriatric psychiatry comes in.
In this post, we’ll explore what geriatric psychiatry is, the most common mental health issues in older adults, warning signs to watch for, and how families can support aging loved ones through expert care.
What Is Geriatric Psychiatry?
Geriatric Psychiatry is a medical specialty focused on the mental health of older adults, typically those aged 60 and above. Geriatric psychiatrists are trained to address the complex interaction of aging, mental illness, medical conditions, and medications.
Unlike general psychiatrists, geriatric psychiatrists are equipped to treat:
Late-life depression and anxiety
Dementia and cognitive decline (e.g., Alzheimer’s disease)
Delirium
Psychosis in the elderly
Substance use disorders in seniors
Behavioral issues due to neurological conditions
They also understand how age-related conditions — like chronic pain, stroke, or grief — can impact mental health.
Is mental illness a normal part of aging?
No, mental illness is not a normal part of aging. While older adults may face life changes such as retirement, grief, and physical health challenges, developing a mental health disorder like depression or dementia is not inevitable. These conditions should be identified and treated, not dismissed as “just part of getting old.”
How is a geriatric psychiatrist different from a regular psychiatrist?
A geriatric psychiatrist is a medical doctor with specialized training in diagnosing and treating mental health disorders in older adults. They understand how aging, chronic illness, and medications affect mental health and can provide care tailored specifically for seniors. They often collaborate with caregivers and other specialists for a holistic approach.
Common Mental Health Issues in Older Adults
Aging doesn’t automatically mean mental decline. However, seniors are more vulnerable to certain mental health conditions, such as:
Depression
Often misdiagnosed or ignored, depression in seniors can lead to withdrawal, poor appetite, and even increased physical illness.
Anxiety Disorders
Concerns about health, finances, or the future may trigger generalized anxiety or panic attacks in older adults.
Dementia & Alzheimer’s Disease
Cognitive issues like memory loss, confusion, and behavioral changes often stem from neurodegenerative diseases.
Delirium
Sudden confusion or disorientation, especially during hospital stays or after surgeries, may signal delirium.
Substance Misuse
Seniors may misuse prescription drugs or alcohol, especially if they’re dealing with loneliness or pain.
Warning Signs Families Should Never Ignore
Recognizing mental health issues in seniors can be difficult because symptoms often overlap with physical illness or aging. Watch for:
Sudden mood changes or irritability
Withdrawal from social activities
Unexplained fatigue or insomnia
Forgetfulness or repeating questions
Poor personal hygiene
Talking about death or hopelessness
Paranoia or delusions
If these behaviors persist, it’s time to consult a healthcare provider — ideally a geriatric psychiatrist.
How Geriatric can Psychiatrists Help?
Geriatric psychiatrists use a holistic approach that includes:
Comprehensive assessments (physical, mental, and emotional)
Medication management to avoid harmful drug interactions
Therapy or counseling tailored for seniors
Family education and support
Coordination with primary care and neurologists
In many cases, treatment can dramatically improve quality of life, restore independence, and ease the burden on caregivers.
What Are the 3 D’s of Geriatric Psychiatry?
In geriatric psychiatry, the “3 D’s” refer to Delirium, Dementia, and Depression — the most common and significant mental health conditions affecting older adults. Recognizing and distinguishing between these conditions is critical for accurate diagnosis and effective treatment.
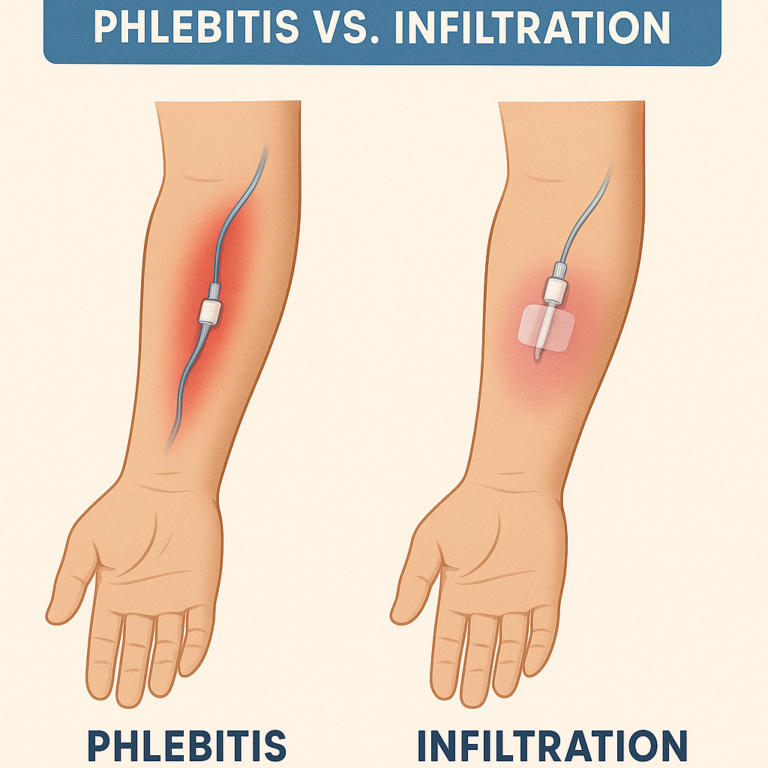
Delirium
Delirium is a sudden and severe change in mental status, often characterized by confusion, disorientation, and difficulty focusing. It typically has a rapid onset and is often reversible when the underlying cause — such as infection, medication reaction, or surgery — is treated. Delirium is a medical emergency and must be addressed promptly.
Dementia
Dementia is a progressive and irreversible decline in cognitive function, including memory, judgment, language, and reasoning. Alzheimer’s disease is the most common type, but other forms include vascular dementia and Lewy body dementia. Unlike delirium, dementia develops slowly over time and significantly impacts daily living.
Depression
Depression in older adults is often overlooked but can be severe and even life-threatening. It may present with symptoms like persistent sadness, fatigue, appetite changes, sleep disturbances, and lack of interest in activities. It is treatable with medication, therapy, or both — but it must first be recognized.
How Families Can Support Mental Wellness in Seniors
You don’t need to wait for a crisis. Here’s how to be proactive:
Talk openly about feelings and mental health
Encourage routine checkups — both medical and psychiatric
Promote social interaction through community programs or hobbies
Watch for warning signs and document any changes
Reduce stigma by normalizing therapy and mental health treatment
Involve a geriatric psychiatrist early when issues arise
Final Thoughts
Mental health is just as important as physical health, especially as we age. Geriatric psychiatry offers hope, healing, and dignity for older adults who may be struggling silently.
If your loved one is showing signs of emotional or cognitive decline, don’t assume it’s just “old age.” There is help — and more importantly, there is hope.
Say Goodbye To Waiting Rooms And Long Lines. Speedy Sticks offers at-home testing.